Is There a Chain of Command in Nursing?

Like the military, nursing has a chain of command to help organize authority. If you have a question or a concern during your shift, to whom do you go? What if you have a problem with a coworker? The answer is determined by your facility’s organizational structure. Understanding the chain of command in nursing will help you navigate life as a professional nurse.
If you have a problem at work, it’s essential to know how to escalate it up the chain of command. Nurses and other clinical staff may need to do this for several reasons:
- Patient safety concerns
- Workplace harassment or bullying
- Staffing issues impacting patient care
- Ethical dilemmas
- Patient or family violence
- Communication breakdowns
- Patient or family complaints
What Is a Chain of Command in Nursing?
The nursing chain of command is a structured hierarchy that outlines the authority, communication channels, and responsibilities within a healthcare organization’s nursing staff. Medical facilities require a clear structure for efficient decision-making and quality patient care.
As a general rule, a nursing chain of command begins with patient-facing staff, such as RNs, LPNs, and CNAs, progressing to charge nurses, unit managers, and non-patient-facing administrators. The higher up the chain progresses, the more systemic authority a person has. But inversely, they’re less likely to interact with patients.
Systems like these rely on everyone understanding their role and trusting each other to do good work. In fact, nurse-manager trust has been shown to boost nurses’ performance. Having confidence in your manager could make you a more effective clinician.
Nursing isn’t the only area you’ll see a chain of command. If you’ve worked at a restaurant, you probably had shift managers and restaurant managers. A clear system for communication and authority helps complex systems — from restaurants to hospitals — run smoothly.
The Importance of Chain of Command in Nursing
Why is chain of command important in nursing? These systems serve several purposes, including:
- Clear lines of authority. The nursing chain of command establishes a clear, hierarchical structure of authority, outlining who reports to whom within each department. This clarity is crucial for efficiency and accountability.
- Communication channels. The chain of command facilitates effective information flow. It defines communication pathways, so that the right people get the right information.
- Roles and responsibilities. Each position in the nursing chain of command comes with specific roles and responsibilities. From top-level executives to frontline staff, understanding one’s role within the hierarchy helps hold everyone accountable.
- Teamwork and collaboration. While the word “hierarchy” isn’t always associated with teamwork, having explicit roles and goals helps everyone function better as a team. Clear delineation of roles allows nursing professionals to work together seamlessly, using their strengths for the benefit of patients.
- Decision-making. In critical situations, quick and decisive decisions are essential. The nursing chain of command enables rapid responses by providing a framework for who should take the lead in various scenarios.
Chain of Command Chart for Nurses
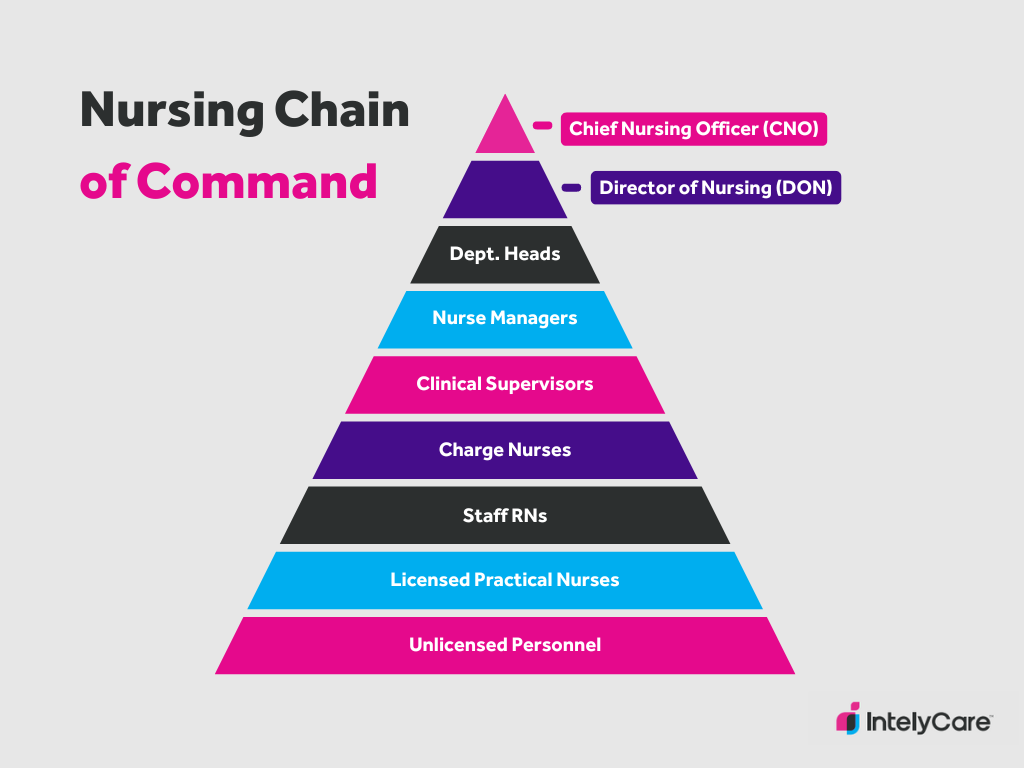
Titles and hierarchy can differ depending on your specialty and the size of your facility, but you’ve probably seen some of the following titles at work:
- Chief nursing officer (CNO): Oversees the entire nursing department, providing strategic leadership and ensuring high standards of patient care.
- Director of nursing (DON): Manages the overall nursing staff and services, offering leadership, supervision, and direction.
- Department heads: In large hospital systems, nursing departments may be divided up by specialty, such as cardiology, pulmonology, and critical care. These leaders focus on supporting their departments and assisting managers in running their units.
- Nurse managers: Oversee specific units or departments, managing day-to-day operations and nursing staff, and ensuring adherence to standards. Some facilities may use night shift managers as well, to add another layer of authority at night.
- Clinical supervisors: Advise nursing staff on appropriate patient care, supporting staff and leading unit education. These nurses might also serve as charge nurses.
- Charge nurses: Have unit authority from shift to shift, making staffing assignments, performing administrative tasks, and assisting other nurses with patient care.
- Staff RNs: Have assigned patient loads, implement care plans, and communicate with the medical team and other interprofessional team members.
- Licensed practical nurses: Have assigned patient loads, delivering patient care under the supervision of RNs.
- Unlicensed personnel: CNAs (certified nurse aides), GNAs (geriatric nursing assistants), and unit secretaries assist with non-medical care tasks, perform administrative to-dos, and help nurses carry out the plan of care.
This nursing chain of command doesn’t run in a vacuum. Nurses interact with the medical team, hospital leadership, and other specialty teams like case management and physical therapy. If you encounter a problem with a staff member from another department, you may need to interact with their chain of command. For example, if a resident isn’t responding to your calls, you’ll need to escalate the problem up both the nursing and medical leadership chain.
Additionally, some nurses work outside of this chain of command. A nurse practitioner who works on the critical care team is part of that team’s structure and does not generally answer to the unit manager or supervisors.
Example of Chain of Command in a Nursing Home
Leadership systems can run differently depending on your facility, but here’s an example of chain of command in nursing homes or skilled nursing facilities:
- Director of nursing
- Assistant director of nursing
- Unit manager
- Charge nurse
- LPN/LVNs
- CNAs
- Patient care assistants
Example of Nursing Chain of Command: Hospital
- Chief nursing officer
- Director of nursing
- Nurse manager
- Charge nurse
- Staff RNs
- CNAs & unit secretaries
How to Use the Nursing Chain of Command at Work
How should you use the chain of command when a problem occurs? Use these three examples to guide your thinking:
- Sarah, an RN, is working a night shift when she notices that a vital piece of equipment on her unit is malfunctioning, potentially compromising patient safety. Despite reporting the issue to the charge nurse, the problem remains unresolved, posing an ongoing risk. Sarah calls the night shift supervisor, emphasizing the urgency of the problems and its potential impact on patient safety.
- Alex, an LPN, has been noticing consistently disrespectful behavior from a clinical supervisor on his unit. It’s affected his quality of life at work, and makes him wonder if he should leave this job. He reports the problem to his unit manager, who has worked with the supervisor for a long time, but the manager doesn’t address the problem. Alex then reports the problem to his department supervisor, who calls a meeting to address all staff members involved.
- Corbin, an RN, is attempting to discharge a patient to a home health team. He’s called the unit social worker several times without an answer. The patient has now been waiting several hours, and is threatening to leave without his discharge paperwork. Corbin alerts his charge nurse, who calls the social work team supervisor to ensure the patient receives their discharge plan promptly.
Looking for New Career Opportunities?
Communication, effective leadership, and responsibility are paramount to a functioning chain of command. In nursing, leadership has a big impact on your ability to do great work. If you’re in the market for a new nursing opportunity, sign up for personalized job notifications.
