The Importance of Data Security in Healthcare: FAQ and Best Practices

The importance of data security in healthcare is increasingly evident as data breaches continue to rise across the industry worldwide. According to one cybersecurity study, 66% of healthcare organizations reported experiencing a ransomware attack, nearly doubling the number of attacks in prior years. Of these organizations, 61% reported feeling obligated to pay the attackers.
To address leadership’s imperative to protect healthcare data security, we’ll share the real organizational costs of breach incidences. We’ll also review five best practices for ensuring data privacy and security in healthcare to help you better safeguard patient information at your facility.
Cybersecurity in Healthcare
Data theft is on the rise in healthcare. Patient information is particularly valuable because it includes not only highly sensitive medical data, but also identifiers (such as name, address, Social Security number) and billing information. Research shows that on the dark web, stolen healthcare data sells for 10 times more than credit card numbers alone.
The impact of cyberattacks on healthcare can be devastating for individuals whose information is compromised. For organizations, the financial implications and loss of public trust are severe. The cost to repair a data breach in healthcare is almost three times higher than in other industries. Yet estimates reveal that only 4-7% of a healthcare system’s information technology (IT) budget is devoted to cybersecurity.
Healthcare Data Security FAQs
In order to prevent cybersecurity attacks, it’s important to understand the basics of healthcare data security. Below we’ll answer some of the most frequently asked questions about sensitive patient information, data protection, and security breaches.
What is security in healthcare’s information landscape?
Information security involves maintaining the confidentiality, integrity, and availability of sensitive patient data, or protected health information (PHI). In particular, the Health Insurance Portability and Accountability Act (HIPAA) establishes national security standards for how PHI should be handled.
In order to uphold information security and comply with HIPAA guidelines for healthcare professionals, facilities must implement a number of physical, administrative, and technical safeguards that protect patient data. Safeguards that impress the importance of data security in healthcare include:
- Facility access
- Workstation controls
- Device security
What is HIPAA and data security’s significance in EHR systems?
Electronic health record (EHR) systems have brought many advances to the delivery of healthcare services. Patient portals make accessing information more convenient than ever, transforming patients into active players in managing their care. However, our reliance on EHRs has also put patient data security at higher risk — a risk specifically addressed by the HIPAA Security Rule — introducing new healthcare data security and compliance challenges. Here are a few statistics about the prevalence of security lapses:
- From 2005 to 2019, 249.09 million people were affected by healthcare data breaches.
- In 2019 alone, over 41 million records were exposed to information breaches.
- During the COVID-19 pandemic, the U.S. healthcare industry reported a 25% increase in successful cyber-security attacks.
What is the organizational importance of data privacy in healthcare?
Beyond compliance considerations, the financial impacts of data breaches are significant. In the U.S., each cyberattack incurs an average cost of nearly $10 million, and the costs don’t stop there.
The effect on the public’s trust in the healthcare system is even more costly. Patients expect that their most personal and confidential information will be kept safe from privacy invasions. That’s why preventing data security breaches is crucial to maintaining professional integrity, protecting patients, and preventing significant costs.
What happens if a security breach occurs?
The HIPAA Breach Notification Rule requires covered entities and their business associates to provide notification following a breach of unsecured protected health information. A patient data security breach can include loss, theft, or the impermissible use or disclosure of unsecured PHI. In the event of a breach, the facility must notify the affected individuals and the U.S. Secretary of Health and Human Services. If the breach affects more than 500 people from a state or jurisdiction, the organization must also notify the media.
Healthcare Data Security Standards and Best Practices
Given the increasing challenges around data privacy and security, you’re likely wondering, What are some ways to maintain security of health information? Here are five best practices for protecting patient information while reinforcing the importance of data security in healthcareworkplace culture.
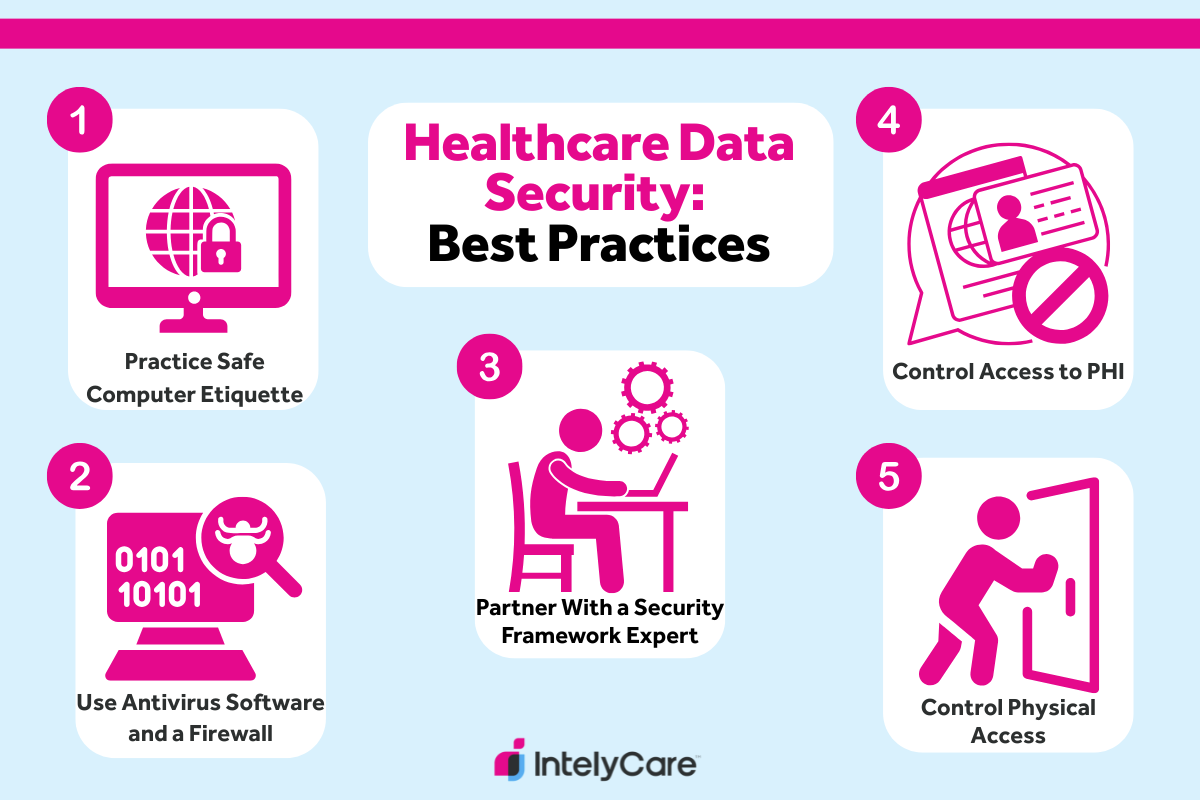
1. Practice Safe Computer Etiquette
Effective security practices don’t have to be expensive. In fact, many are completely free. They’re simply personnel habits that may take time and effort to establish. For example, workstations should be locked at all times when unattended, even if the person intends to step away for only a moment.
Developing a culture of safety around healthcare data security can help mitigate data privacy risks through teamwork. The more staff watch out for each other, monitoring for areas of concern, the more likely they are to identify issues and proactively address them. A team member strongly committed to the importance of data privacy in healthcare would notice an unattended workstation and take steps to log the user off or lock the computer.
Additional Considerations:
- Use computer privacy screens to prevent accidental privacy lapses.
- Perform regular software maintenance and updates.
- Reinforce the importance of never downloading unapproved software.
2. Use Antivirus Software and a Firewall
These systems work together to protect your facility from external internet threats. Antivirus software destroys and prevents the spread of malware while a firewall prevents it from gaining access to your computer systems. A virus can allow outside users to steal or destroy data and take control of your computer — jeopardizing health information safety and patient data security.
Installing a firewall and antivirus software can be complicated and will likely be configured and maintained by your IT department. But all staff need to be aware of the dangers of malware and know how to recognize a computer that might have become infected with a virus.
Additional Considerations:
- Streamline the process for reporting suspicious computers to IT.
- Develop policies that define and support safe computer use.
- Educate staff through training on additional healthcare data security risks, like use of local area networks (LANs), internet browsing, and external email systems.
3. Consider Partnering With a Security Framework Expert
Specialized frameworks, created by security experts specifically for the healthcare industry, can provide a structured, verified approach to healthcare data security and risk management. Programs like these build on regulatory requirements like the Privacy Rule (HIPAA’s guideline for who can access PHI and how) to protect patient and organizational data security.
Although hiring a consulting firm can be costly, there are many alternative methods of strengthening your cybersecurity. However it’s done, investing in data defense measures is a tangible demonstration of an organization’s commitment to the importance of data security in healthcare.
Additional Considerations:
- While shopping for new EHR platforms, consider prioritizing systems that offer a vendor alliance or the opportunity for upgraded security options.
- Partner with other local healthcare institutions to run collaborative, low-cost cybersecurity education events.
- Leverage your health information exchange (HIE) partnerships to gain discounted group security coverage.
4. Control Access to Protected Health Information (PHI)
The highly sensitive nature of healthcare information requires strict compliance with patient data security measures. Establishing and adhering to an access control system is one strategy for protecting PHI. Access to information in the EHR should be limited to a “need-to-know” basis, defined by each employee’s roles and responsibilities.
Another method of ensuring compliance is through routine auditing of information access, with follow-up data reviews. In addition to the IT department, your data governance committees will be involved with oversight and making updates to role-based access control recommendations.
Additional Considerations:
- Educate staff on HIPAA standards to avoid an unintentional, costly violation. Training instructions should include the severity of ramifications for HIPAA noncompliance.
- Reinforce the importance of data security in healthcare by establishing ongoing check-ins for data governance committees within new employee mentoring meetings.
- Immediately terminate access for all employees who leave employment. All badges, IDs, and tracking/access devices are to be collected on the employee’s last day.
5. Control Physical Access
The most common way that electronic health information is compromised is through lost devices. Many organizations now issue certain staff members laptops and mobile devices in addition to all of the electronic devices, network servers, and computers that remain on site. All of these carry the risk of being lost or stolen, compromising the information they contain.
For institutions that support medical research, managing data can be even more tedious. One recommendation for those sorts of organizations is to create a data enclave, which can help ensure a secure, yet collaborative environment. This would help reinforce keeping the clinical, patient environment limited exclusively to those who need to be there, protecting security starting at the first, physical level.
Additional Considerations:
- Arrange the environment so that access points for healthcare data (such as computers) are separate from public areas with heavy visitor traffic.
- Ensure devices with EHR access are secured between use by keeping them in locked cabinets (preferrably with badge access for staffing convenience).
- Regularly inventory health data storage and management devices to quickly identify lost or missing equipment.
Looking for More Ways to Keep Patient Data Secure?
Knowing the importance of data security in healthcare, you may feel inspired to revitalize your own patient privacy protections. IntelyCare can help. Tackle any of your latest healthcare goals with our diverse range of expert-driven facility guides and recommendations.
IntelyCare writer Katherine Zheng, PhD, BSN, contributed to the research and writing of this article.

