What Is the APRN Consensus Model? Nursing Guide

The APRN consensus model in nursing is a framework for creating nationwide regulations in the licensure and practice of advanced practice registered nurses (APRNs). Initially proposed in 2008 by the National Council of State Boards of Nursing (NCSBN), it advocates for a standardized licensure process and full-practice authority in every state.
APRNs are nurses who have obtained additional education, completing a master’s, post-graduate, or doctoral degree in nursing practice. Their additional training allows them to treat patients under an expanded scope of practice. They can order tests, prescribe, diagnose, and much more.
APRNs include:
- Nurse practitioners (NPs)
- Certified nurse midwives (CNMs)
- Clinical nurse specialists (CNSs)
- Nurse anesthetists (CRNAs)
APRNs are increasingly essential in nearly every setting — from primary care to the operating room. Yet there’s still no nationwide agreement on the amount of supervision they need from physicians, their licensure requirements, or their practice scope. Instead, these parameters fall to individual state boards of nursing and can be found in their respective Nurse Practice Acts. That’s where the model for APRN consensus comes in.
Understanding the Consensus Model for APRN Regulation
The model is a set of standards and recommendations endorsed by over 40 nursing organizations and professional groups. It defines what an APRN is, what their titles are, the populations they treat, baseline requirements for their education, and standards for new specialties as they emerge.
There are seven main parts of the model:
- Defining the Advanced Practice Registered Nurse as a nationally recognized title
- Outlining the certification and licensure requirements of an APRN
- Listing the four APRN roles
- Outlining minimum postgraduate requirements for all APRNs
- Requiring the passage of a nationally accredited certification exam for all APRNs
- Granting independent practice authority to all APRNs, without physician oversight
- Granting independent prescriptive authority to all APRNs, without physician oversight
One of the focuses of the model is to address APRN practice misalignment. The majority of NPs, for example, are educated and certified in primary care, yet they may work in a variety of specialty settings. Less than half of PICUs, for example, require that NPs hold acute care certification. This misalignment can lead to liability for NPs and risk for patients.
Similar to the RN licensure compact, this model aims to create uniform standards for APRNs, with required specialty tracks. With full implementation of the model, APRNs would be able to treat patients across state lines more easily and practice in different states without completing additional state licensure applications.
APRN practice legislation is a complex system. Each state has licensure requirements that generally include a national certification from an organization like the American Academy of Nurse Practitioners (AANP). These certifying organizations require specific education, and other organizations, like the Commission on Collegiate Nursing Education (CCNE), determine whether schools are educating students appropriately. Because of this complexity, the model doesn’t require immediate implementation, but anticipates a gradual rollout of policies.
What Are the Four Main Elements of the Consensus Model?
The model requires buy-in from four different organization types. It recommends that boards of nursing, school accrediting organizations, certification programs, and educational programs each adopt the following practices.
1. Licensure
Boards of nursing will:
- Be solely responsible for licensing APRNs in all four categories within a specific population focus.
- Only license graduates of accredited graduate programs that apply APRN core competencies, as outlined in the model.
- Require national certification that assesses core competencies for licensure.
- Not issue temporary licenses; APRNs will only be licensed when education and certification are complete and congruent.
- License APRNs as independent providers with no regulatory requirements for collaboration, supervision, or direction.
- Allow mutual state recognition of APRNs through an APRN Compact.
2. Accreditation
Organizations that accredit NP educational programs will:
- Be responsible for evaluating APRN programs, including graduate and post-graduate degrees.
- Evaluate programs using established accreditation standards and core APRN competencies.
- Assess developing education programs and new education tracks using the above process, potentially granting pre-approval, pre-accreditation, or accreditation prior to student enrollment.
- Include an APRN on the visiting team when a program is being evaluated.
- Monitor education programs during the accreditation period.
3. Certification
APRN certifying bodies will:
- Follow established standards for licensure examination.
- Assess APRN core and role knowledge across at least one population focus.
- If appropriate, assess specialty competencies separately from the core role and population focus.
- Be accredited by a national certification accreditation body.
- Apply congruence between education programs and certification exams.
- Provide pathways to ensure continuing competency and certification maintenance.
- Make the certification processes transparent to the boards of nursing.
- Communicate with state boards of nursing and schools of nursing.
4. Education
APRN education programs will:
- Follow established standards to ensure that students obtain APRN core competencies.
- Be accredited by an organization recognized by the U.S. Department of Education (USDE) and/or the Council for Higher Education (CHEA).
- Obtain pre-approval, pre-accreditation, or prior accreditation when accepting students to all new education tracks.
- Ensure that program graduates are eligible for national certification and state licensure.
- Provide transcripts that specify the role and population focus of the graduate.
Consensus Model Pros and Cons
What do leaders and APRNs like and dislike about the model? These are some potential benefits and drawbacks.
| Pros | Cons |
|---|---|
| Greater alignment between educational programs, certifications, and roles could mean better NP-driven care in specialty settings.
APRNs would be able to work in more critical access areas, where patients already rely on them for care. Clearer role delineation can reduce confusion about the APRN scope, specialty areas, and education. |
The model may force FNPs currently working in a specialty to acquire additional education and certification to continue practicing.
Slow adoption of the model means that the U.S. is far behind initial goals. Some physicians believe that increased autonomy for NPs may mean that patients receive less team-based care. |
APRN Consensus Model by State

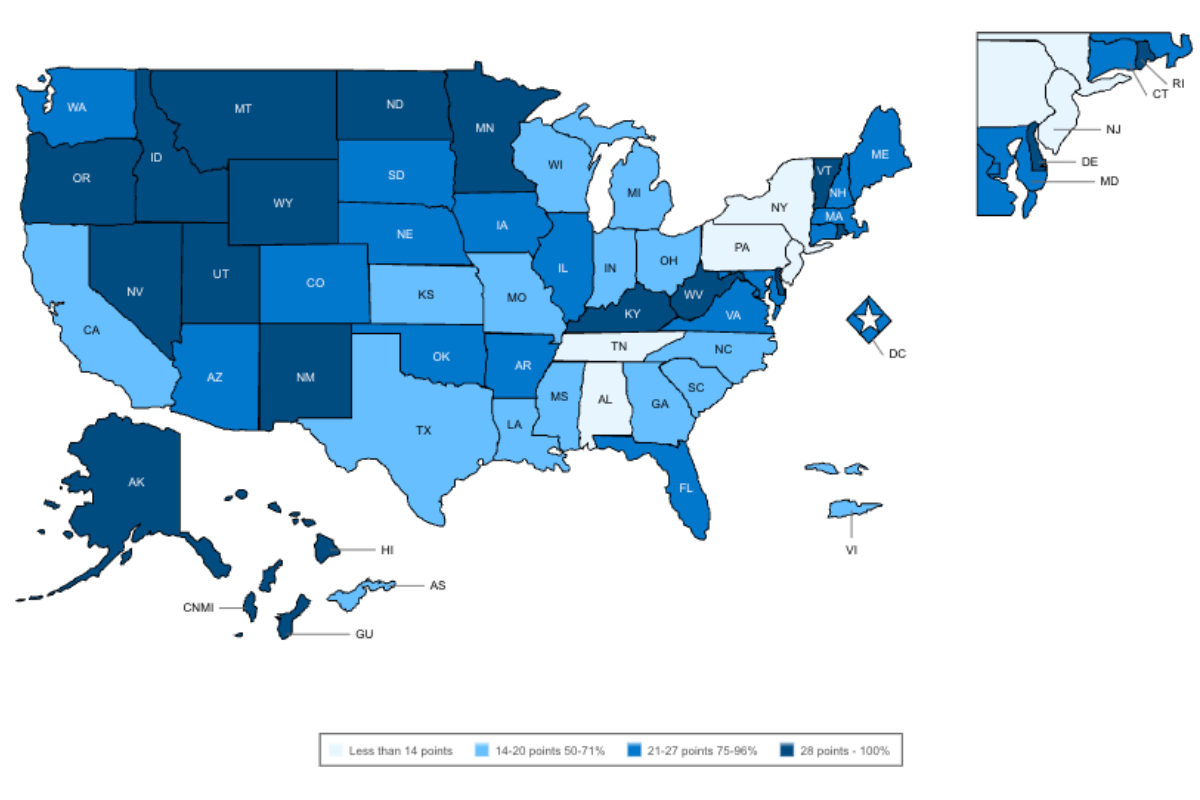
The map above displays the consensus model implementation status of U.S. states and territories, based on the NCSBN’s scoring grid.
FAQ
Is an APRN considered a doctor?
No. While some advanced practice nurses have doctoral degrees (DNPs or PhDs), they are not physicians and have a more narrow practice scope. To avoid patient confusion, it’s generally recommended that NPs not introduce themselves as doctors. Learn more about the differences between NPs and doctors.
How much do APRNs make?
These are the average annual salaries for APRN roles:
- CRNA salary: $231,700
- NP salary: $132,000
- CNM salary: $128,110
- CNS salary: $105,206
What can an APRN not do?
It depends on where they live and work. In general, limitations on APRNs fall into these categories:
- Prescriptive authority: In some states, APRNs can’t prescribe certain medications, like controlled substances, without oversight from a physician.
- Independent practice: Many states require a partnership or oversight from a physician to diagnose, manage, and treat patients.
- Specialty scope: APRNs must practice within their certified population focus. For example, a neonatal NP wouldn’t treat adult patients without additional training.
Find Roles for APRNs
Whether you work in a state that has adopted consensus model standards or not, your skills as an APRN are vital. If you’re seeking a new role or just curious about what’s out there, we can help. Learn about personalized job notifications that alert you to roles that fit your specialty, location, and schedule.