Nursing Home Case Study: Increasing Reimbursements

How IntelyCare Helped an Ohio Facility Improve Documentation & Increase Reimbursement
Ensuring proper clinical documentation among nursing staff is critical for post-acute care organizations to maximize CMS reimbursement. A skilled nursing facility in Ohio knows this all too well as it was experiencing documentation issues with the Certified Nursing Assistants (CNAs) working in its building. Improper documentation led to a rise of “Do Not Returns” (DNRs) among IntelyCare’s nursing professionals (“IntelyPros”), but it quickly became evident that the problem was pervasive across all full-time and agency staff at the organization.
Working with the Director of Nursing, the IntelyCare Quality Assurance (QA) team began to identify a root cause residing in the facility’s instance of PointClickCare. This software system is the central point where the facility holds data. The platform allows nursing professionals to easily record care and notes from patient to patient and visit to visit. Due to the customizable nature of the system, an error occurred when setting up the system that was causing CNAs to miss a critical step in documenting the care they provided.
Digging in further, IntelyCare discovered log-in issues with the system, resulting in undocumented downtime, and issues with assignment changes, where residents were switched due to acuity, but the changes went undocumented. Here’s a deeper look at this nursing home case study and the ways that IntelyCare adds real value for its partners.
Better Documentation Leads to Higher Reimbursements
While CNA documentation doesn’t have a direct one-to-one relationship with reimbursement, it is critical. Proper documentation affects the amount of reimbursement a facility receives because it helps to determine acuity and the amount of time needed to care for a patient. CNAs are often the ones to record the data that can drive further assessments and interventions by the care team.
For instance, CNAs record Activities of Daily Living (ADLs) which includes things such as bathing, eating, dressing, and toileting, as well as the patient’s ability to participate in these activities, or the time spent helping with these activities. If a CNA documents that a patient has difficulty ambulating, or that a patient reported pain, then the nurse would further assess and potentially notify the provider or provide treatment within their scope. In addition, if it’s documented that a patient didn’t eat, and then that their blood sugar reading is low, a nurse would titrate the amount of insulin they dose and might notify a provider to review insulin orders or request a nutrition consult.
Centers for Medicare and Medicaid (CMS) has very strict rules around reimbursement so if you didn’t document it, it didn’t happen, and the facility cannot bill — or be reimbursed — for that level of care.
Scaling the Solution to Support Long-Term Care
In our ongoing commitment to help our partner communities achieve their workforce goals, IntelyCare’s QA team solves problems fast and digs in to ensure they’re fixed for the long-haul. We don’t want to just provide a short-term solution, but instead to partner with organizations so that we can make systemic improvements to avoid issues in the future.
In situations like this nursing home case study, IntelyCare can also use these learnings to improve our other clients’ workflow. This discovery made at this facility had far-reaching implications for the greater community of IntelyCare’s partners and we decided to double down on our efforts to improve documentation of care. The IntelyCare team used the learnings from the issue with this PointClickCare setup and advised other clients to review their systems.
In addition, we built in additional messaging and documentation reminders for our IntelyPros to make sure that documentation was always a focus of care. IntelyCare also pays IntelyPros their hourly rate to return to a facility for missed documentation.
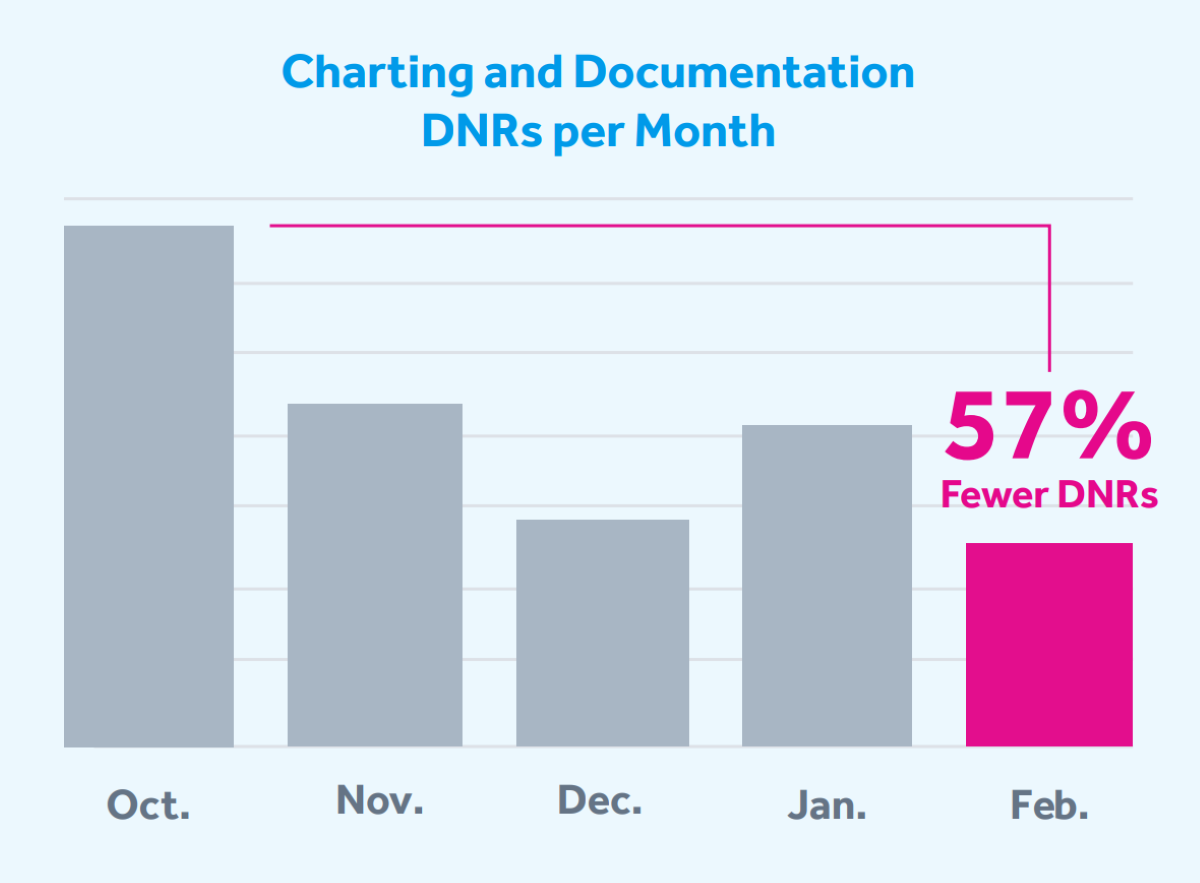
Finally, we improved our training with an emphasis on documentation, which is mandated for every IntelyPro. The training has resulted in a 57% reduction of documentation-related DNRs across all our clients in just five months.
Partnering to Deliver a Higher Quality of Care
IntelyCare employs a Quality Assurance team of former DPH/DOH auditors, long-term care directors of nursing, and long-term care staff nurses. The QA team is always available to assist our partners whenever there is an incident or allegation with one of our IntelyPros. They’ll conduct a workplace investigation, follow up directly with administration and clinical leadership, and take the steps necessary to ensure it doesn’t happen again.
Ready to Increase Your Reimbursements?
Whether it’s improving documentation and reimbursements or helping to fill shifts with qualified nursing professionals, this nursing home case study shows that IntelyCare never stops finding ways to add value for our partners. Find out how we can help you get the most out of your staffing strategy today.
