EHR Optimization for Nursing Leaders

Could your facility use some help with recordkeeping? EHR optimization is the process of refining, streamlining, and customizing electronic health records (EHRs) to better support clinicians and improve patient care. Optimizing an EHR means considering how it’s used and continuously working to make the system suit clinical workflows. But what does the process look like? Learn more about improving EHR systems for staff and patients.
What Is EHR Optimization?
Electronic health records, commonly referred to as EHRs (and sometimes also called electronic medical records, or EMRs), are digital systems for recording, communicating, and organizing information about patients and their care. They are notoriously complex because they serve multiple stakeholders at once — clinicians, billing departments, administrators, regulatory bodies, and IT teams all rely on the same platform for different needs. This results in systems packed with features, menus, alerts, and documentation requirements.
If you’ve ever had to check multiple boxes for one assessment finding, you’ve experienced an EHR system that needs optimization. Little redundancies or inefficiencies add up when nurses are taking care of several patients a shift, leading to more time on the computer and less time at the bedside.
As a nurse leader, you can use a well-optimized EHR to reduce burnout symptoms, improve safety, and ensure that clinical documentation supports both patient care and regulatory standards.
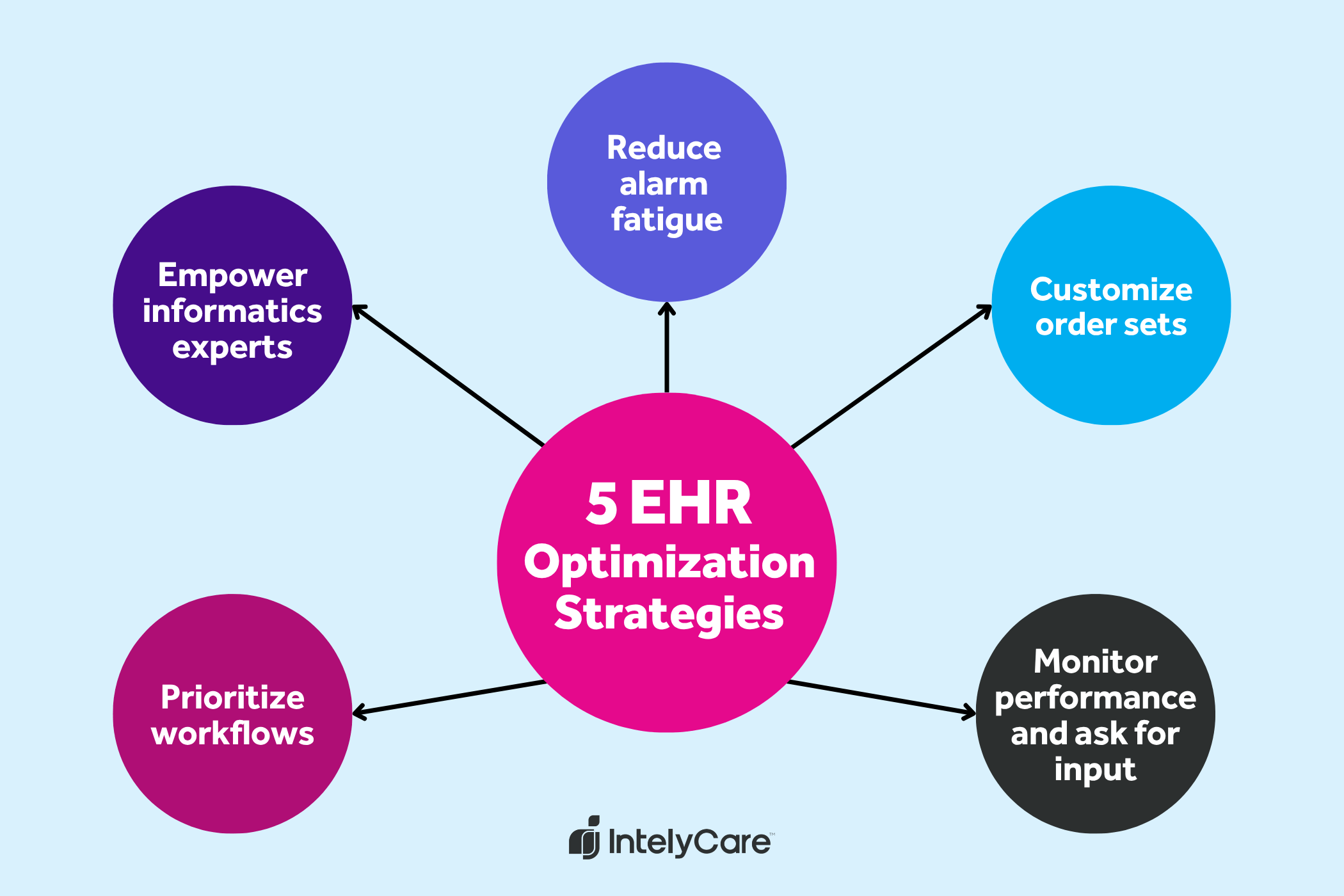
5 EHR Optimization Strategies for Nursing Leaders
Because EHR systems are so complex, it can be hard to know where to put your improvement efforts. In addition to providing EHR training for your staff, use the five strategies below.
1. Prioritize Workflows
Review and simplify documentation templates — especially flow sheets and reassessment forms — to reflect actual clinical processes. For example, on an inpatient psychiatric unit, nursing staff are not likely to perform a full cardiac assessment on every shift, so it’s wise to omit this section in routine documentation. A case study showed that redesigning nursing assessment flowsheets cut documentation time by over 18% and reduced reassessment documentation time by up to 97%.
2. Empower Superusers and Informatics Experts
Identify the experts who are here to help and the staff who are motivated to learn. EHR specialists like nurse informaticists are indispensable when making systematic tech improvements. Staff nurses who are willing to become superusers are also major assets when testing changes, training others, and relaying feedback. Involving nurses directly helps ensure that adjustments are practical, user-friendly, and focused on patient care needs.
3. Reduce Alarm Fatigue
Tailor alert sensitivity to reduce alarm fatigue and help staff prioritize. In ICUs, an average of 43 alarms ring out every hour, and only about 6% relate to clinical physiological changes. Over 42% of alarms go unanswered. Reducing alarms as much as possible can help staff respond when they need to, reduce unit noise, and keep patients safer.
4. Customize Order Sets
Whenever possible, reduce the number of decisions your staff needs to make. Simplify and curate order sets so they reflect best practice guidelines without adding unnecessary steps. For example, when chemotherapy is prescribed for a patient on an oncology unit, the EHR may auto-trigger a specific EHR workflow to implement chemo precautions, nutrition needs, and more.
5. Monitor Performance and Ask for Input
Evaluation is an essential part of the nursing process. Before, during, and after optimizing your EHR system, ask for staff input to gain insight on how they use different elements. Measure compliance with process changes, and approach challenges with curiosity. A growth mindset is the best asset wherever you’re in the EHR workflow optimization process.
EHR Optimization Plan: 4 Steps
Even minor improvements to your electronic health record system can have a big impact on clinical workflows, nurse satisfaction, and patient outcomes. The exact plan for improving your EHR system will vary based on your facility, the expertise you have access to, and other factors. In general, you can start by using the following process:
Step 1: Assessment
The first step is assessing the current state of EHR use. Begin by gathering feedback directly from your nursing staff. This can include satisfaction surveys, workflow observations, time audits, and click counts for common tasks. Ask nurses where they experience bottlenecks, frustrations, or inefficiencies. Prioritize issues that negatively affect patient safety, quality of care, or staff well-being.
Step 2: Build a Team
Next, build a multidisciplinary optimization team. This should include frontline nurse users, nurse informaticists or super users, IT representatives, and clinical leaders. Ideally, it also includes voices from quality and safety teams. Nurses should play a central role in these discussions, because they know the workflows best and will use the system after improvements.
Step 3: Pilot, Measure, and Iterate
From there, break down the changes that need to be made and identify one area upon which to improve. For example, you might streamline pain reassessment documentation, reduce non-actionable alerts, or revise handoff templates using an SBAR format. Choose a unit or small team to test the change. Throughout the project, track usage data, collect feedback, and refine based on what works and what doesn’t.
Step 4: Scale and Sustain
Once a change proves successful at a small scale, expand it across additional units or departments. Support implementation by training staff and providing clear communication about why changes are being made and what the goal of improvements is. Staff may resist change, especially at first. Be patient, and recruit change agents to help drive improvements.
Optimization is an ongoing process. Continue to measure the impact with metrics like nurse satisfaction, EHR usability, chart audit results, or relevant safety indicators. Set up systems for getting feedback from staff, and adjust workflows as new clinical needs emerge or EHR capabilities evolve.
Improve Your Unit With Improved Staffing
EHR optimization is just one part of what makes a great nursing unit. If you’re seeking a new work setting, opportunities are closer than you think. Our personalized job notifications will alert you to roles that fit your scheduling, specialty, and location needs. Learn more today.