With high rates of burnout and turnover among healthcare workers, facilities are facing serious headwinds to maintain minimum staffing levels and remain profitable.
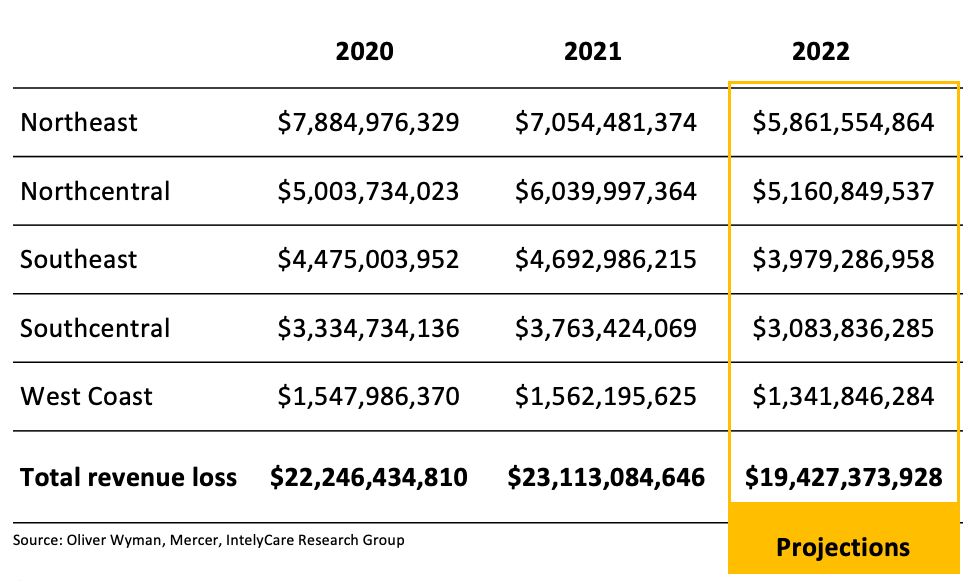
The post-acute care industry is estimated to have $19.5BN in unrealized revenue by the end of 2022. Why? The current shortage of nursing staff in the U.S. is hitting the post-acute care space hard, making it extremely difficult to maintain the staffing levels needed to increase occupancy and drive organizational funding and reimbursement.
In “The True Cost of Post-Acute Care Labor,” global management consulting leader Oliver Wyman examines the financial impact that the nurse staffing crisis is having on facilities and how contingent nursing labor can be utilized to combat it.
Every unoccupied bed represents a loss of revenue for a healthcare facility and the inability to increase patient referrals is hitting post-acute care space particularly hard. Occupancy rates in some U.S. regions have dropped to nearly 60% from the 72% to 87% averages seen between 2015-2019.
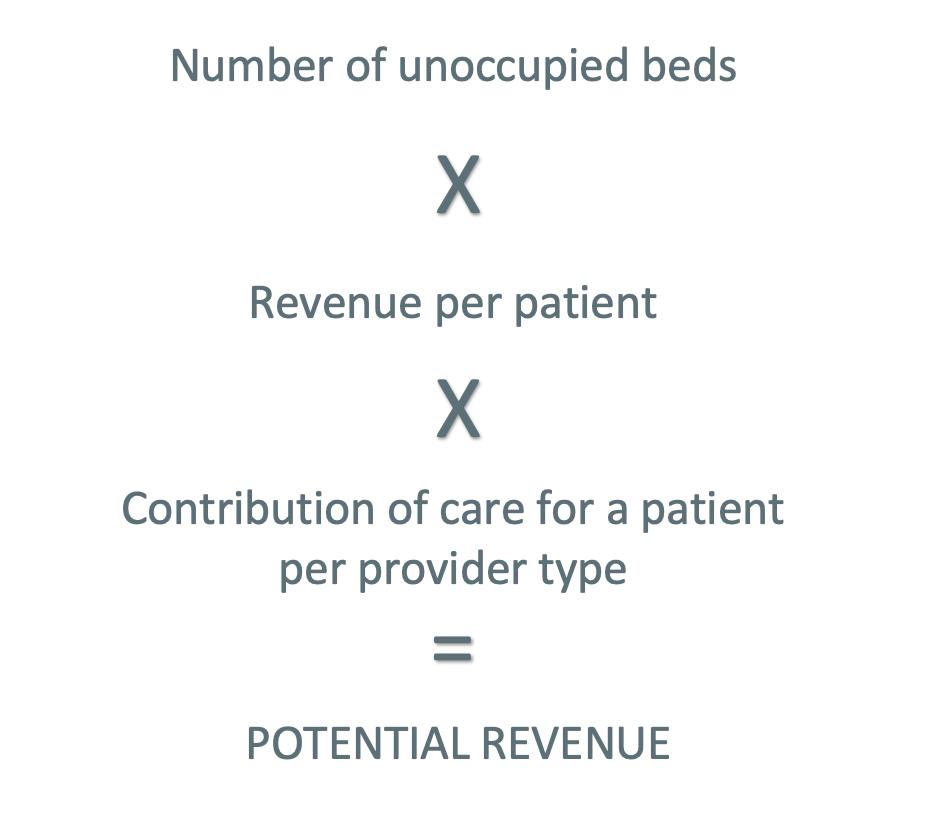
Oliver Wyman calculates lost revenue as follows:
Despite slight rebounds towards pre-pandemic norms in 2022, there is still a significant gap from pre-COVID occupancy. More facilities are being forced to turn away referrals due to the lack of staffed beds and are unable to capture this potential revenue.
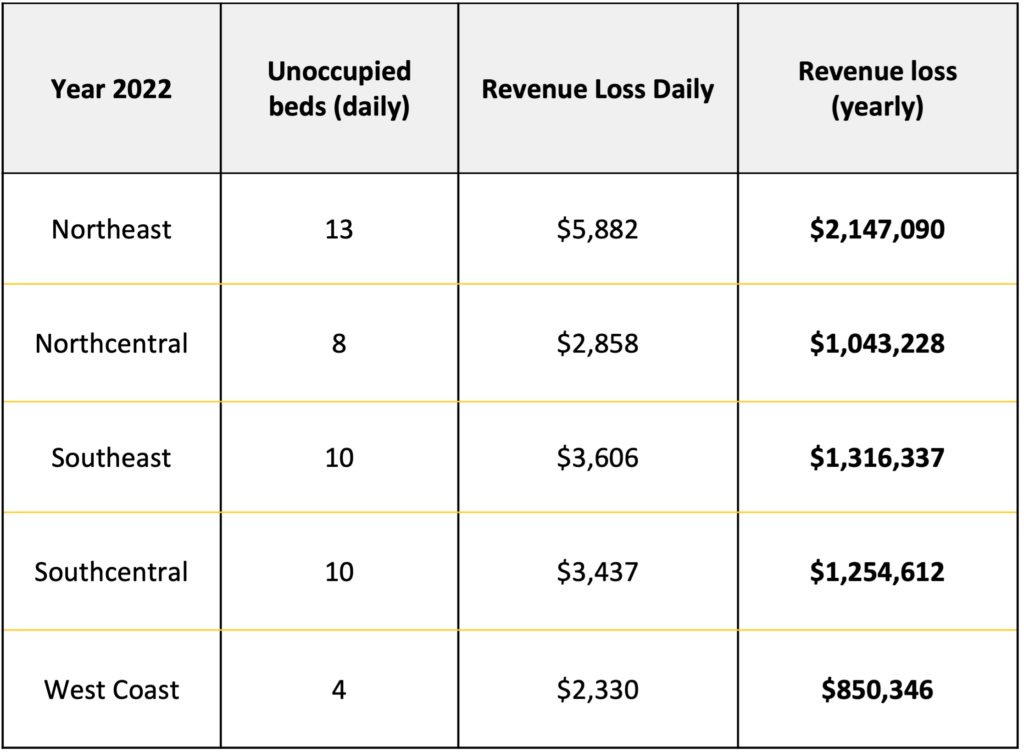
On a per facility basis, an average facility is expected to lose anywhere from $2,300 to nearly $5,900 per day due to staffing shortages. This represents up to $2.1MN a year in lost revenue for the most affected region – the Northeast.
The post-acute care market is undeniably in a staffing crisis fueled by the ongoing COVID-19 pandemic. More nurses and nursing assistants are leaving healthcare than ever before. Some are leaving altogether; others are leaving full-time positions in search of more flexible, part-time opportunities.
Contingent labor is often perceived as a temporary solution that is far less preferable than staffing a facility with full-time employees. However, Oliver Wyman’s research shows that this may be a harmful perception. In many cases, contingent labor is less expensive, more flexible, and less resource-intensive to a facility than identifying, recruiting, and retaining new full-time talent.
Want to learn more?

