What Is the Revenue Cycle in Healthcare? Facility Guide and FAQ

Tracking and receiving payments is necessary in order for organizations to maintain financial stability. For healthcare facilities, however, this process isn’t as straightforward as charging patients a fixed fee. This may leave you wondering, What is the revenue cycle in healthcare? Because of the way health insurance claims play into service delivery, facilities must take unique measures when managing their financial processes.
In this article, we’ll help you understand the stages of the healthcare revenue cycle so that you can work to optimize it at your facility. Effective management of the cycle, from start to finish, is vital to operating a financially successful organization.
In addition to breaking down the revenue cycle definition in healthcare, we’ll also answer frequently asked questions and give you three practical strategies that you can implement at your facility today.
What Is the Revenue Cycle in Healthcare?
The healthcare revenue cycle refers to every step of the care process that goes into calculating how much a patient should be billed. This cycle begins with a patient’s initial encounter at a facility to the time that payments for services are received in full. Throughout the healthcare revenue cycle process, facilities track essential pieces of information that influence patient revenue, such as:
- Patient medical histories
- Health insurance payers
- Medical diagnoses and codes
- Approvals and denials of claims
What Are the 13 Steps of Revenue Cycle Management?
When reviewing the revenue cycle definition in healthcare, it’s important to consider all steps of the process. The overarching structure can be broken down into three stages, each with several steps. Taken as a whole, the revenue cycle process in healthcare is more complex than in other industries, and entails many chances for error.
Proper management of each step is crucial for ensuring your facility is compensated for services rendered. As we break down each step, consider the ways your facility implements it currently and think about potential ideas for improvement.
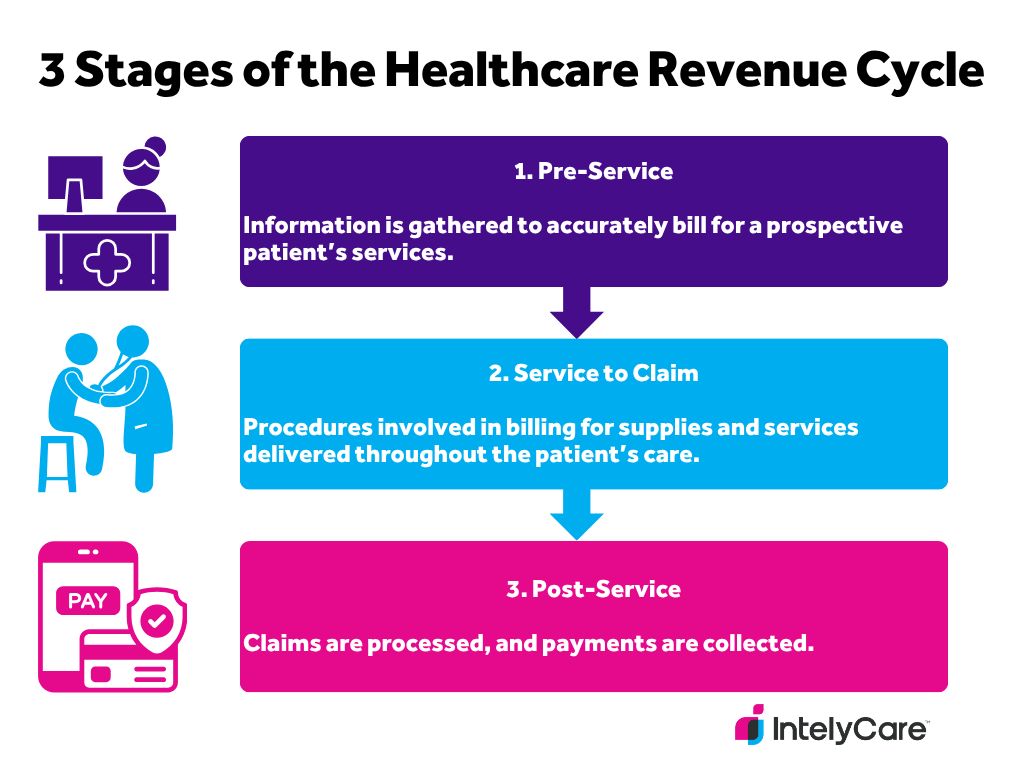
First Stage: Pre-Service
The first stage involves gathering the information needed to accurately bill for a prospective patient’s services. Here’s a closer look at the steps involved:
- Pre-registration and/or registration: Administrators gather all relevant contact information, medical records, and insurance information.
- Verification of insurance coverage: Staff members take measures to verify that insurance information is accurate and up-to-date. They may check coverage details and discuss out-of-pocket costs with the patient.
- Pre-authorization: Staff members may seek pre-authorization from an insurance provider for some procedures and services to prevent later claim denials.
Second Stage: Service to Claim
The second stage includes all of the procedures involved in billing for supplies and services delivered throughout the patient’s care. This is an important stage, since codes need to accurately reflect the services that were administered.
- Patient encounter: The patient receives services from a care provider. During the encounter, the provider and all staff involved document services rendered.
- Medical transcription: The documentation of the services administered is converted into documentation that details all procedures, treatments, and supplies that can be billed for.
- Medical coding: The documentation is used to generate ICD-10 and CPT codes.
- Claims generation:Medical billers review ICD and CPT codes, fixing any errors to generate a bill for medical insurers. Claims are submitted to insurers or government payers.
Third Stage: Post-Service
During this final stage, claims are processed and payments are collected.
- Claims management: Payers determine and communicate their financial responsibility for the claim. They may offer full or partial reimbursement, or deny the claim.
- Denial management: Staff may investigate denied claims, and appeal the denial to seek resolution.
- Patient billing: Patients are billed for the remainder of what is owed to the facility.
- Payment processing: Staff documents payments received from the patient and payer, and reconciles differences.
- Collections: Staff follows up with patients regarding installments on flex payment plans and balances due.
- Reporting: Staff tracks relevant financial data and shares it with stakeholders and facility leaders.
What Does the Healthcare Revenue Cycle Management Process Look Like in Practice?
Now that we’ve answered the question, What’s the healthcare revenue cycle? in theory, we’ll also look at how this process unfolds in the real world. To get a better idea of how the revenue cycle works in a typical healthcare setting, take a look at a simplified example below.
|
|
|
|---|---|
|
1. Pre-Service |
Mr. Smith schedules his annual exam through a local clinic’s online appointment portal. He uploads his medical history, insurance, and contact information. A receptionist reviews and verifies this information, also calling Mr. Smith’s insurer to double check his eligibility for coverage. |
|
2. Service to Claim |
Mr. Smith comes into the office for his checkup. His doctor documents this wellness exam into Mr. Smith’s patient chart on the EHR system. An ICD code for Mr. Smith’s diagnosis and CPT codes for his exam procedures are automatically generated. |
|
3. Post-Service |
After Mr. Smith’s visit, medical billers review the ICD and CPT codes in his chart alongside his insurance plan. They send a bill over to his insurer, which approves and pays for the coverage costs. Mr. Smith is then sent a bill for any other uncovered costs, which he pays via credit card through his online portal. |
Why Is Revenue Cycle Management Important?
Every type of business should understand the revenue cycle and implement strategies for managing each stage. So, why is it important to healthcare organizations specifically? If facilities collect incorrect information or carry out improper billing practices, they may lose out on revenue. Moreover, proper revenue cycle management can also help improve workflow and care delivery, allowing facilities to:
- Keep patients more informed about their care costs.
- Avoid overcharging or undercharging patients and insurers.
- Minimize delays and costs resulting from denied insurance claims.
- Facilitate communication between administrative and clinical staff.
- Bridge gaps between healthcare providers, billers, and insurers.
What Is the Healthcare Revenue Cycle’s Relationship to Patient Satisfaction?
Your facility’s billing processes heavily influence a patient’s experience with your business, which extends beyond a clinical visit. A confusing, clunky, outdated, or error-prone revenue cycle may cause frustration and dissatisfaction for patients. This is particularly true for the post-service stage, when patients must navigate facility billing procedures to settle their account balances. In contrast, convenient billing options and friendly communication can go a long way toward developing trust and loyalty.
What Are Effective Strategies For Healthcare Revenue Cycle Management?
When it comes to revenue cycle management, healthcare facilities can explore different ways to streamline the collection, review, and submission of payment information. Your exact process for managing the revenue cycle will depend on the types of services you provide and the patients you serve. However, facilities can follow these general tips to improve their processes.
1. Automate Repetitive Tasks
Technology is rapidly advancing in the healthcare industry, providing many opportunities to automate repetitive administrative and care-related procedures. If your facility primarily relies on manual coding or billing, explore ways to adopt electronic systems that automatically link medical and administrative information.
2. Engage and Train Your Staff
While technology can help streamline billing processes, your staff plays an important role in overseeing these procedures. Provide regular training on any new technologies you decide to adopt. Additionally, engage your staff by soliciting ongoing feedback on what types of resources can support workflow.
3. Consider the Patient Experience
Patients also play an important role in the revenue cycle, meaning it’s important to make your services as accessible as possible. Implement efficient and effective ways to collect information and payments from patients without burdening them.
This may involve providing different options for how patients complete their intake forms, such as uploading their information online or filling out packets in-office. Also, consider accepting multiple payment modes (e.g., credit card, debit card, check, cash) to make the collection process more inclusive.
Discover More Ways to Enhance Your Services
Now that you can answer the question, What is the revenue cycle in healthcare? you may have more questions about your facility’s financial operations, compliance efforts, and patient care practices. We’re here to support you with expert tips to improve your patient care services — from intake to discharge, and every phase in between.

